#6 Blog: How do you do? Mental Health during the COVID-19 Lockdown
The COVID-19 lockdown, for many of us, was more than a huge challenge. On the one hand, people had to cope with social isolation. On the other hand, there were multiple burdens households with children faced - managing childcare, home office and the closed educational and care facilities, just to mention a few. States of emergency are expected to leave traces in mental health conditions. Thus, our “Multiple Burdens during COVID-19” survey also included questions measuring the mental health status of Austrians during the COVID-19 lockdown.
The questions for determining the general mental health status were based on the depression module of the Patient Health Questionnaire Depression Scale (PHQ-D). This is a valid and widely used tool for the identification of mental disorders in clinical practice and research (Gräfe et al. 2004). In our survey, we made use of the depression scale (PHQ-8), consisting of eight diagnostic criteria. However, the application of individual modules, such as the depression module, as we do it, has a screening function rather than a diagnostic function (Löwe et al. 2002, Gräfe et al. 2004). The eight criteria of the PHQ-8 depression module are as follows:
Little interest or pleasure in doing things
Feeling down, depressed, or hopeless
Trouble falling asleep or staying asleep, or sleeping too much
Feeling tired of having little energy
Poor appetite or overeating
Feeling bad about yourself - or that you are a failure or have let yourself or your family down
Trouble concentrating on things, e.g. reading the newspaper or watching television
Moving or speaking so slowly that others could have noticed; or rather being so 'fidgety' or restless that you have been moving around a lot more than usual
To measure each of the eight items, we asked eight separate questions in the survey. Each question, of whether one felt impaired by a specific problem during the last two weeks could be answered with "Never" (0 points), "On single days" (1 point), "More than half of the days" (2 points) and "Nearly every day" (3 points). In addition to categorical diagnosis, the depression module allows dimensional evaluation (such as sum scores with cut-off values) to determine severity levels of problems (Renn et al. 2008). A higher score-sum, thus, indicates more pronounced mental stress.
Our analysis of the average number of points across all eight diagnostic dimensions yields an average value of 6.5 points. For women, the average score is 6.8, that is slightly above average, while for men, the average score is 5.2, that is slightly below the average. And the analysis by household type reveals that single parents, with an average score of 8.7, are way above the average, while couple households without children score lowest, with an average score of 5.5. For all other household types, couple households with children under 15 years of age, single households, and other household types (e.g. multi-generational households or shared flats) the score is close to the average, ranging from 6.6 to 6.8.
In addition to the general state of mental health during the lockdown, we assessed whether the symptoms had improved, worsened or remained unchanged compared to the situation before the COVID-19 lockdown. Figures 1 and 2 show the proportion of people who reported a worsening, improvement or no change in their symptoms, evaluated by gender and household type.
Crisis management at the expense of women's (mental) health?
We find a strikingly clear picture in the gender differences in mental health (see Figure 1): The share of women who reported that their problems had worsened during the lockdown is higher than the share of males, reporting a worsening, in each of the eight diagnostic categories. Males, however, reported more often that their health status remained unchanged compared to the situation before the COVID-19 lockdown. The difference in the share of women and men reporting a worsening is particularly pronounced in the categories B. Melancholy (16%), E. Changes in appetite (11%) and A. Little interest in/pleasure from doing things (12%).
Figure 1: Change in mental health (PHQ-8) compared to the situation before the lockdown by gender
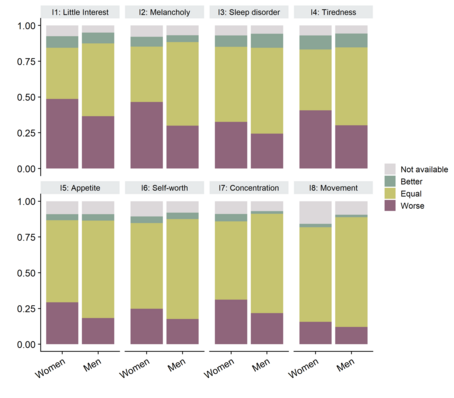
This figure shows changes in the diagnostic criteria according to the PHQ-8 scale during the COVID-19 lockdown as compared to before the lockdown. Source: Multiple Burdens under COVID-19 Survey; Own Representation, 2020.
Single parents and couples with children particularly affected
The evaluation of mental stress by household type reveals worrying patterns (Figure 2): In all dimensions, single parents reported a worsening of their complaints as compared to before the COVID-19 lockdown. In 7 out of the 8 dimensions, about half (between 42% and 63%) of the single parents we surveyed reported their condition had worsened. In addition, a high share of parents living in couple households with children under 15 years of age, said their mental health was worse during than before the lockdown, in particular in the dimension A. Little interest or pleasure in doing things; B. Feeling down, depressed, or hopeless and D. Feeling tired of having little energy.
In addition, a relatively share of single households reported a deterioration in their situation - particularly in areas C. Trouble falling asleep or staying asleep, or sleeping too much and E. Poor appetite or overeating. The least affected group in terms of deteriorating health conditions, across all categories, is couples without children under 15 years of age. In general, improvements in mental health have been rarely reported in most diagnostic categories. However, in categories C. Trouble falling asleep or staying asleep and D. Feeling tired of having little energy, 10% of people living in couple households without children (under 15 years of age) and single households without children reported improved conditions. But this is, however, outweighed by the (worryingly) high fraction of people reporting a worsening in their conditions. The high share of women and parents with children under 15 years of age reporting a deterioration of their mental health during the lockdown indicates the difficulties these groups of people were facing during the lockdown.
Figure 2: Change in mental health (PHQ-8) compared to the situation before the lockdown by household type
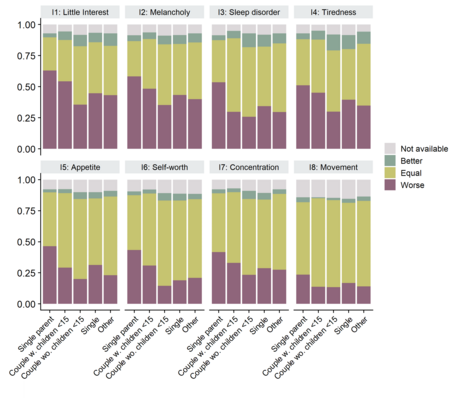
These figures shows changes in the diagnostic criteria according to the PHQ-8 scale during the COVID-19 lockdown as compared to before the lockdown. Source: Multiple Burdens under COVID-19 Survey; Own Representation, 2020.
Figure 3: Agreement with the statements on "Reconcilableness of family and work during home office" by gender
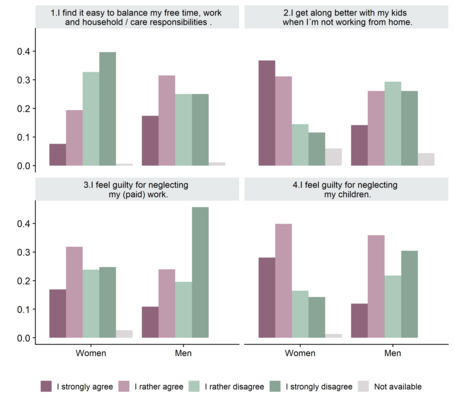
The questions leading to items 1 to 4 in Figure 3 was distributed only to persons with children under the age of 15 years, who, during the COVID-19 lockdown worked (at least from time to time) in home-office. Source: Multiple Burdens under COVID-19 Survey; Own Representation, 2020.
Difficulties and feelings of guilt in the reconciliation of family and work
Due to the necessity to organise (paid) home office work, childcare, home schooling and domestic work, such as cooking and cleaning, made the lockdown particularly difficult for people with children (under 15 years of age). Thus, in what follows, we are having a closer look at the situation of parents who worked at least partly in home-office during the lockdown.
In our survey, we asked this group of persons about their approval or rejection of four selected statements on the topic of "Reconcilableness of family and work during home-office”, and the results are shown in Figure 3. There you can see the proportion of persons who, strongly agree, rather agree, rather disagree, or strongly disagree with the four statements by gender. Apparently, there is, first, a large difference by gender. For example, almost ¾ of women (72.4%) rather or strongly disagreed with statement 1 (“I find it easy to balance my free time, work and household/care responsibilities”. Males, by contrast, strongly or rather disagreed in “only” half of cases. And the share of respondents who fully agree that this is an easy task is more than twice as high as for men (17.4%) than for women (7.6%).
The gender differences in the answer to statement 2 "I get along better with my children when I leave home for work and do not work in the home office” are substantial as well. Almost 70% of women rather (36.7%) or fully (31.2%) agreed with this statement, while the agreement is much lower among males (14.1% fully agreed; 26.1% rather agreed). The answers to statements 3 and 4 “I feel guilt for neglecting my (paid) work / my children” highlight that women in particular suffered from feelings of guilt - both, in the area of paid work and with regard to their children. Roughly 50% and 70% of women fully or rather agreed to statement 3 and four, respectively, while these values are significantly lower for men, that is, 35% and 50%, respectively.
The results of our survey point to the difficult situation of women and persons living in households with children under 15 years of age during the COVID-19 lockdown: these groups disproportionately reported a deterioration of their mental health status (see Figures 1 and 2). As explained in our previous blog posts, both before and during the lockdown, the burden of unpaid work, in particular childcare and home-schooling, falls on women. The reconciliation of paid and unpaid work during the COVID-Lockdown was hard in particular for women and went hand in hand with feelings of guilt towards neglecting paid work and children (see Figure 3).
Literature
Gräfe, Kerstin/ Zipfel, Stephan/ Herzog, Wolfgang/ Löwe, Bernd (2004): Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)“. Diagnostica 50, Nr. 4: 171–81.
Löwe, Bernd/ Spitzer, Robert L./ Zipfel, Stephan/ Herzog, Wolfgang (2002): Gesundheitsfragebogen für Patienten (PHQ-D). Manual und Testunterlagen (2. Auflage). Karlsruhe: Pfizer.
Renn Daniela/ Höfer, Stefan/ Schüßler, Gerhard/ Rumpold, Gerhard/ Smrekar, Ulrike/ Janecke, Nicola/ Doering, Stephan (2008). Dimensionale Diagnostik mit dem Fragebogen zur Erfassung von DSM-IV-Persönlichkeitsstörungen (ADP-IV). Z Psychosom Med Psychother 54, 214–226.
